Understanding NF2 >
NF2 Tumors
Last Updated: 05/9/25
Index
1. Tumor Development2. NF2 Tumor Types by Location
- Bilateral Vestibular Schwannoma
- Additional Brain Tumors
- Spine Cord Tumors
- Peripheral Nerve Schwannoma
- Skin Surface
4. Tumor Descriptions
5. NF2 Tumor Growth Variables:
- Treatments / Food / Envirnment
6. Sources
Also See
Schwann Cells and Nerve Damage1. Tumor Development
The condition NF2:SWN results in the growth of different tumor types. NF2 tumors are and typically remain benign (noncancerous). Each NF2 tumor type can result in serious damage as a result of what each tumor grows on or near, and tumor malignancy (cancerous) is a possibility with tumors over a few centimeters.
Based on an individual's exact NF2 mutation (variation), tumor development follows a typical pattern, even if the tumor growth rate and development can increase or decrease at some rate due to life choices. The mutation, however, is the biggest part of the tumor growth pattern.
In individuals with NF2, tumors grow along the peripheral nervous system (PNS) and along the spinal cord [Plotkin, 2012] typically have a slower rate of growth than brain tumors.
2. NF2 Tumor Types by Location
Tumors might be a combination of; schwannoma (neurilemoma), meningioma, or ependymoma. Tumor formation types can develop, including some combination of the following five (5) locations:
Risk percentage noted is based on a study of 58 adults in a study done at Massachusetts General Hospital, in 2012. [3]
Tumors at the Intercranial/Crebellopontine angle of the brain:
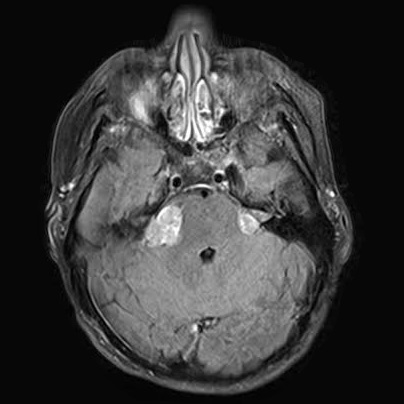
Bilateral Vestibular Schwannoma (VS), Acoustic Neuroma (AN)
- Tumor growth on both, the left and right, vestibulocochlear nerve (Cranial Nerve 8), hearing/balance nerves, and possibly the facial nerve (Cranial Nerve 7).
- A schwannoma is an overgrowth of a schwann cell.
- Approximately 98% of people with neurofibromatosis type 2 (NF2) develop bilateral VS tumors.
Additional Intercranial Tumors:
Schwannoma, Meningioma, and Ependymoma
- Schwannoma on Cranial Nerves: (37%)
Schwannoma growth in the brain is rarely limited to just the Vestibular Nerves - Intracranial Meningioma: (54%)
Meningioma can easily develop throughout the brain - Spine:
Spinal Ependymoma
Spinal Cord Tumors:
Schwannoma (58%), and Ependymoma (38%)
Peripheral Nerve Schwannoma:
Schwannoma (37%) and possibly Neurofibroma (>1%) on nerves outside of the brain and spine
Skin Tumors (Cutaneous Lesions)
- Cutaneous Schwannoma, (Dermal Schwannoma): (38%)
- Subcutaneous Schwannoma: (27%).
NF2 Diagnostic Criteria as of 2018
Note #3 - Neurofibroma: There is a rare occurrence of neurofibroma tumors in individuals with NF2.[Tumors displaying hybrid schwannoma and neurofibroma features in patients with neurofibromatosis type 2, 2016]
Note #1 - Café-au-lait Macules: Skin Irregularities: Café-au-lait Spots also known as Café-au-lait Macules (CALMs), are irregularities of the skin that could cover a 1-inch area. These are not painful; they are simply a discoloration of the skin. Individuals with NF2, who have CALMS, usually have fewer than six. CALMS can also fade over time.
Note #2 - Tumors Types and Tests: It is not possible to tell the difference between schwannoma, meningioma, or neurofibroma in an MRI. Schwannoma and Meningioma are easily identifiable in surgery. The difference of either schwannoma or neurofibroma with tumor biopsy.
3. NF2 Tumors and Skin Irregularities
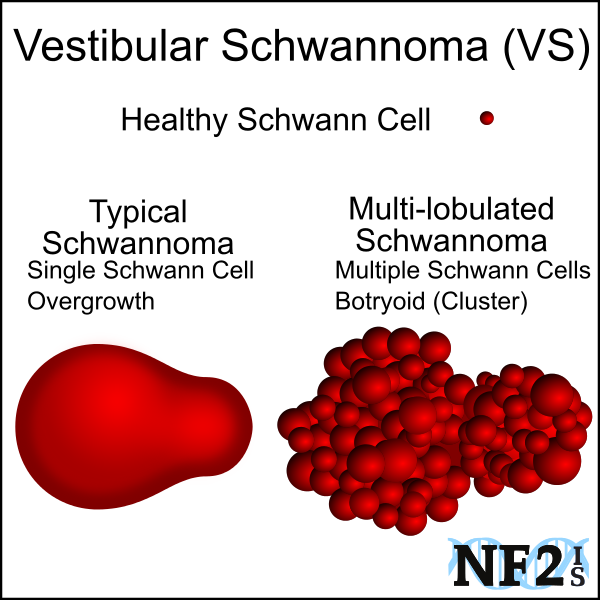
(Acoustic Neuroma)
(Typical vs. Multi-lobulated)
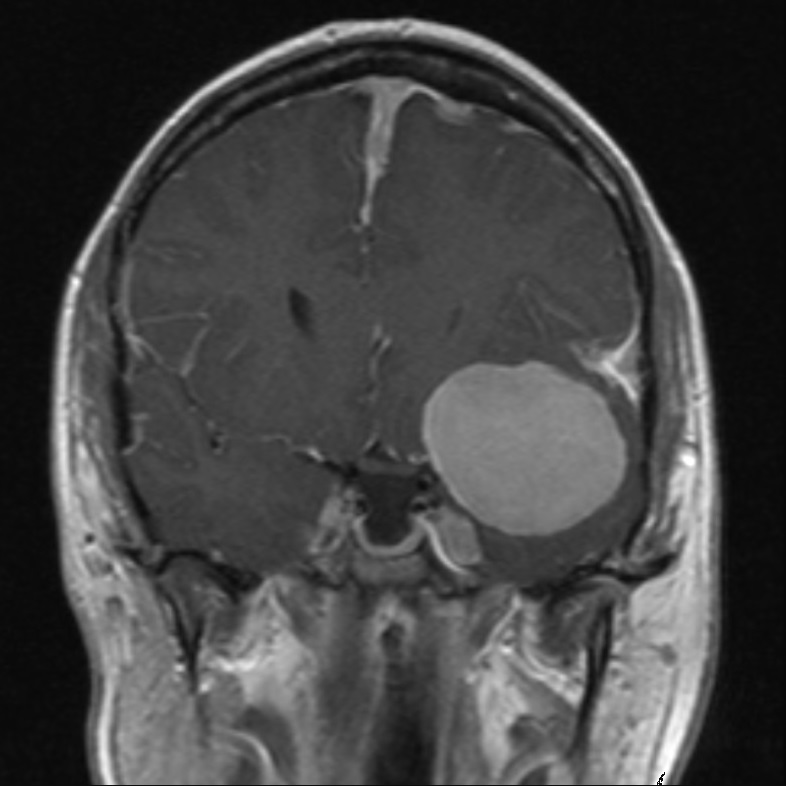
Meningioma
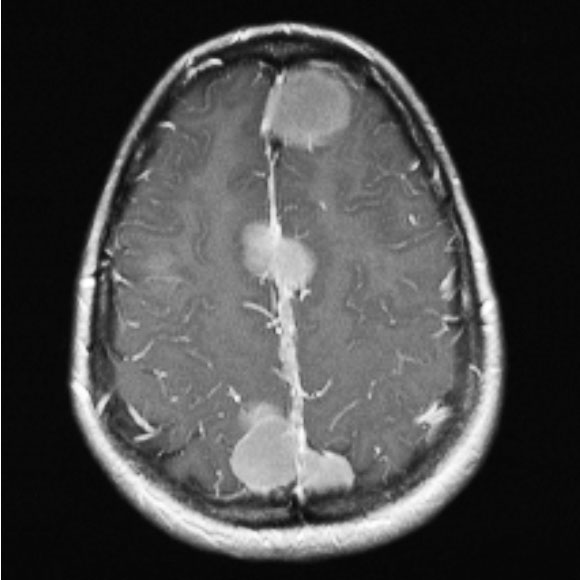
Undetermined Cranial Tumor -
Meningioma or Schwannoma
Lower Spine (Lumber)
Schwannoma
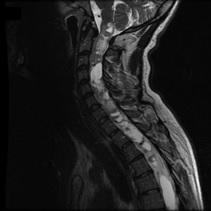
Upper Spine (Cervical)
Ependymoma

Cutaneous Tumor
(part of tumor over skin surface)
Subcutaneous Tumor
(tumor under skin)
Cafe Spot
(not a tumor - skin discoloration)



4. Tumor Descriptions
Schwannoma (Neurilemmoma or Neurinoma):
These are typically Benign (Non-cancerous) tumors that are the result of an abnormal overgrowth of a Schwann Cell in nerve cells Myelin Sheath.
- Vestibular Schwannoma (VS), Acoustic Neuroma (AN): The Vestibular Nerve attaches the Vestibule to the brainstem,
between these two points the nerve passes between a bone structure, and because of this results in typically a pear-shaped
mass. Overgrowth of a schwann cell
Schwannoma tumors alone the Vestibular Nerve are not always the result of the condition NF2. For individuals who develop Schwannoma from NF2, the tumors might be either; 1) Typical, which is an overgrowth of one Schwann cell, or 2) Multi-lobed masses which are combined Schwann cells of possibly different parts of the Vestibular Nerve but can be more complex.
- Learn more about VS
- Learn more about Nerves - Central Nerve System Tumors: These are tumors that grow on Cranial Nerves (CN) (nerves within the Brain) and along the Spinal Cord; these are most frequent occurring Schwannoma tumors for NF2.
- Spinal Cord Tumors: Tumors that grow along the Spinal Cord[Plotkin, 2012] have a slower rate of growth than brain tumors.
- Peripheral Nervous System Tumors: Tumors that grow along the PNS (Peripheral Nervous System)
[Plotkin, 2012] have a slower rate of growth than brain tumors. These
are tumors that grow on nerves outside of the Brain and Spinal Cord, and along the rest of the body, there are two
forms of these:
- Cutaneous Schwannoma: These are tumors that can be seen as a bulge just under the skin but are not painful.
- Subcutaneous Schwannoma: These are tumors that can be seen as a bulge just under the skin but are painful.
Meningioma:
Meningioma develop as Encapsulated and Benign Tumors, as these tumors reach different sizes as a result of simple growth or treatment(s) of Radiation. Either way, Meningioma can have dangerous or even fatal consequences, depending on the World Health Organization (WHO). As a tumor grow the classification of the tumor may reach the next grade level and increased not just a tumors WHO grade, as well as speed of growth, but the chance that it will grow back if removed in surgery or may be hard to control with other treatments.[ Tew, 2013]
- WHO Grade 1: When these tumors start to grow they are slow growing, Benign.
- WHO Grade 2: These are Atypical tumors have a higher rate of regrowth if surgically removed.
- WHO Grade 3: These tumors are Malignant / Anaplastic, (irrespective of brain invasion).
Glioma
- Astrocytoma: A type of glial cells that can start to grow in the Cerebrum, but do grow further than the Spinal Cord
- Ependymoma:
5. NF2 Tumor Growth
Tumor growth rates can vary dramatically. Different growth rates are the results of:
- Genetics: Mutation and Natural Life Factors
- Epigenetics: Environmental and Lifestyle
i. Genetics
While genetics play a big role in tumor growth rate, other things can make additional variations on expected growth. Surgery stress and radiation are now accepted reasons for tumor growth, other issues including hormones are also believed to be a factor responsible for increased tumor growth.
As we grow, we create new cells, each with a copy of our original set of DNA. Sometimes this copying process is imperfect, leading to a gene mutation that causes the gene to code for a slightly different protein. Some mutations are harmless, some can be helpful, and others give rise to disabilities or conditions. [NIH. Brain Basics]
ii. Epigenetics: Environmental and Lifestyle
Epigenetics is the process by which gene expression is regulated by events other than alterations of the genome.
Genes are not the only determinants of how our bodies function. Throughout our lives, our genes can be affected by the environment. In medicine, the term environment includes not only our physical surroundings but also factors that can affect our bodies, such as sleep, diet, or stress. These factors may act alone or together in complex ways, to change the way a gene is expressed or the way messages are conducted in the body.
There are different possible Epigenetic reasons for NF2 tumor development, growth rate, and possible change of tumor grade, unrelated to the NF2 mutation type of an individual.
6. Sources
-
Mattson, Mark P., and Simonetta Camandola. "NF-?B in neuronal plasticity and neurodegenerative disorders." The Journal of clinical investigation
107.3 (2001): 247-254.
https://www.jci.org/articles/view/11916 -
Franco-Caspuenas, Sandra, et al. "Uncovering cellular senescence as a therapeutic target in NF2-related vestibular schwannoma." Hearing Research 455 (2025): 109165.
DOI: https://doi.org/10.1016/j.heares.2024.109165 | Source: https://www.sciencedirect.com/science/article/pii/S0378595524002181 -
Yuan, Xingyue, Ruibo Li, and Qian Liu. "Intradural extramedullary double primary ependymoma and meningioma rare condition: Case report and literature review"
Medicine 104(2):p e41210, January 10, 2025.
DOI: 10.1097/MD.0000000000041210 Source: https://journals.lww.com/md-journal/fulltext/2025/01100/intradural_extramedullary_double_primary.42.aspx -
Philips Professional Healthcare. "Spot check vital signs monitoring systems: Respond to changing patient conditions"
Source: https://www.usa.philips.com/healthcare/solutions/patient-monitoring/spot-check-monitoring-systems -
Deora, Harsh, et al. "Rare cranial nerve schwannomas: A retrospective review of nontrigeminal, nonvestibular cranial nerve schwannomas."
Journal of Neurosciences in Rural Practice 9.2 (2018): 258
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5912035/ | DOI: 10.4103/jnrp.jnrp_469_17 -
Tew, John MD. "Meningiomas." Mayfield Brain & Spine. (As of: 2018)
Source: http://www.mayfieldclinic.com/PE-MENI.htm -
Plotkin, Scott R., et al. "Quantitative assessment of whole-body tumor burden in adult patients with neurofibromatosis."
PloS one 7.4 (2012): e35711.
Source: http://dx.plos.org/10.1371/journal.pone.0035711 | DOI: 10.1371/journal.pone.0035711 -
Evans, D. Gareth R., and Sarah Louise Ingham. "Reduced life expectancy seen in hereditary diseases which predispose to early-onset tumors."
The Application of Clinical Genetics 6 (2013): 53.
Source: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3735038/ | DOI: 10.2147/TACG.S35605 -
Dilwali, Sonam, et al. "Secreted factors from human vestibular schwannomas can cause cochlear damage." Scientific Reports
5 (2015): 18599.
Source: https://www.nature.com/articles/srep18599/ | DOI: 10.1038/srep18599 -
National Institutes of Health (NIH). "Brain Basics" (As of: 2018)
Source: http://www.nimh.nih.gov/health/educational-resources/brain-basics/brain-basics.html -
Evans, D. G. "Neurofibromatosis type 2 (NF2): a clinical and molecular review." Orphanet J. Rare Dis. 4, 16 (2009).
https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-4-16 | DOI: 10.1186/1750-1172-4-16 -
Asthagiri, A. R. "Neurofibromatosis type 2." Lancet 373, 1974-1986 (2009).
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60259-2/fulltext | DOI: 10.1016/S0140-6736(09)60259-2 -
Montgomery, Blake K., et al. "Tumors displaying hybrid schwannoma and neurofibroma features in patients with neurofibromatosis type 2." Clinical neuropathology 35.2 (2016): 78.
Source: https://search.proquest.com/openview/49611335ba3062422d42ae93da414d26/1?pq-origsite=gscholar&cbl=2044862 | DOI: 10.5414/NP300895 -
Roussel, Martine F., and Jennifer L. Stripay. "Epigenetic drivers in pediatric medulloblastoma." The Cerebellum (2017): 1-9.
Source: https://link.springer.com/article/10.1007/s12311-017-0899-9 | DOI 10.1007/s12311-017-0899-9 -
"Tumor Grade." National Cancer Institute at the National Institutes of Health (Reviewed: May 3, 2013)
Source: https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis/tumor-grade-fact-sheet -
Evans, D. Gareth, et al. "Identifying the deficiencies of current diagnostic criteria for neurofibromatosis 2 using databases of 2777
individuals with molecular testing." Genetics in Medicine (2018): 1.
https://www.nature.com/articles/s41436-018-0384-y -
Akella, Sraavya S., et al. "Vestibular Schwannoma growth during pregnancy: case report of neurofibromatosis type 2 in pregnancy." (2018): 1.
https://ir.uiowa.edu/cgi/viewcontent.cgi?article=1094&context=pog_in_press -
Supartoto, Agus, et al. "Relationships between Neurofibromatosis-2, Progesterone Receptor Expression, the Use of Exogenous Progesterone, and Risk of Orbitocranial Meningioma in Females." Frontiers in Oncology 8
https://www.frontiersin.org/articles/10.3389/fonc.2018.00651/abstract - Billings, Steven D. "Nerve Sheath and Related Tumors." Soft Tissue Tumors of the Skin. Springer, New York, NY, 2019. 345-381. https://link.springer.com/chapter/10.1007/978-1-4939-8812-9_10 | https://doi.org/10.1007/978-1-4939-8812-9_10
-
Hollon, Todd, et al. "Supratentorial hemispheric ependymomas: an analysis of 109 adults for survival and prognostic factors." Journal of neurosurgery 125.2
(2016): 410-418.
DOI: https://doi.org/10.3171/2015.7.JNS151187 | Source: https://thejns.org/view/journals/j-neurosurg/125/2/article-p410.xml -
Kresak, Jesse Lee, and Meggen Walsh. "Neurofibromatosis: a review of NF1, NF2, and schwannomatosis." Journal of pediatric genetics 5.02 (2016): 098-104.
Source: https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0036-1579766 -
Division of Cancer Epidemiology & Genetics at the National Cancer Institute "Neurofibromatosis Type 1 and Cancer Susceptibility"
Source: https://dceg.cancer.gov/research/what-we-study/neurofibromatosis-cancer-risk -
Plotkin, Scott R., et al. "Updated diagnostic criteria and nomenclature for neurofibromatosis type 2 and schwannomatosis: An international consensus recommendation."
Genetics in Medicine 24.9 (2022): 1967-1977.
DOI: https://doi.org/10.1016/j.gim.2022.05.007 | Source: https://www.sciencedirect.com/science/article/pii/S1098360022007730


 |Google Play
|Google Play